- Politics
- Diversity, equity and inclusion
- Financial Decision Making
- Telehealth
- Patient Experience
- Leadership
- Point of Care Tools
- Product Solutions
- Management
- Technology
- Healthcare Transformation
- Data + Technology
- Safer Hospitals
- Business
- Providers in Practice
- Mergers and Acquisitions
- AI & Data Analytics
- Cybersecurity
- Interoperability & EHRs
- Medical Devices
- Pop Health Tech
- Precision Medicine
- Virtual Care
- Health equity
Deep Learning Model Predicts Risk of Breast Cancer Better than Traditional Practice
The model placed 31% of patients with future breast cancer in the top risk decile, versus the 18% seen with traditional models.
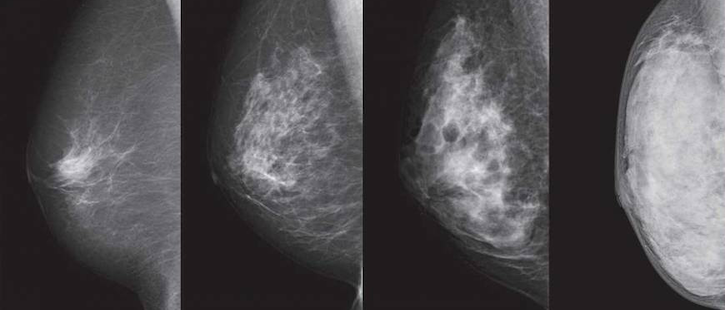
Photo/Thumb have been modified. Courtesy of NPO BREAST CANCER IMAGING NETWORK.
A deep learning model can be used to predict a woman’s future risk of breast cancer better than traditional practice, according to the findings of a study published in the journal Radiology.
The artificial intelligence (AI) model identified women at high risk for breast cancer and placed 31% of all patients with future breast cancer in the top risk decile. This was an improvement over the Tyrer-Cuzick model, which is typically used in clinical practice and was shown to predict risk in just 18% of patients.
Using a hybrid model, the researchers found that patients with non-dense breasts and model-assessed high risk had 3.9 times higher cancer incidence than patients with dense breasts and model-assessed low risk.
While AI models do not always perform well across diverse races, the hybrid model had an area under the curve of 0.71 for both Caucasian and African American women. The traditional model had an area under the curve of 0.62 and 0.45, respectively.
“Until now, African American women were at a distinct disadvantage in having accurate risk assessment of future breast cancer,” said Regina Barzilay, Ph.D., professor at the Massachusetts Institute of Technology (MIT).
Adam Yala, Ph.D. candidate at MIT, along with Barzilay and Constance Lehman, M.D., Ph.D., chief of breast imaging at Massachusetts General Hospital in Boston, compared three risk assessment models: One relied on traditional risk factors, one relied on deep learning that used the mammogram, and one hybrid approach incorporated traditional factors and mammograms. The team developed the models with risk factor information from patient questionnaires and electronic health records to assess breast cancer risks within five years.
Mammograms contain more information than just the four categories of breast density, Yala said. “So what (the model) will do is discover things that are subtle and might not be visible to the human eye, but are truly indicative of cancer risk,” he told Inside Digital Health™ in an interview.
The research team used nearly 89,000 full-resolution screening mammograms from more than 39,500 women between January 2009 and December 2012 to train, validate and test the model. The researchers obtained cancer outcomes through linkage to a regional tumor registry.
By identifying patients at risk early, there is an increased chance of survival due to early intervention.
“We can now leverage these kinds of models to do the discovery for us, and that results in much stronger tools,” Yala said.
Get the best insights in digital health directly to your inbox.
More AI Insights
Tackling the Misdiagnosis Epidemic with Human and Artificial Intelligence
The Artificial Intelligence Question
AI Struggles Across Health Systems, Needs Wide-Range Testing
