- Politics
- Diversity, equity and inclusion
- Financial Decision Making
- Telehealth
- Patient Experience
- Leadership
- Point of Care Tools
- Product Solutions
- Management
- Technology
- Healthcare Transformation
- Data + Technology
- Safer Hospitals
- Business
- Providers in Practice
- Mergers and Acquisitions
- AI & Data Analytics
- Cybersecurity
- Interoperability & EHRs
- Medical Devices
- Pop Health Tech
- Precision Medicine
- Virtual Care
- Health equity
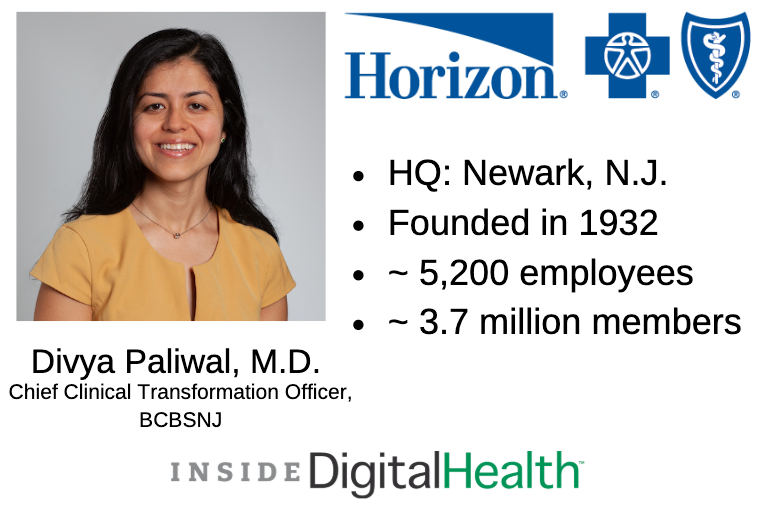
Executive Voices: Divya Paliwal, M.D., Chief Transformation Officer of Horizon BCBSNJ
The chief transformation officer is reshaping how care is delivered to the insurer’s 3.7 million members.
As healthcare continues to change, it's up to the chief transformation officer to keep tabs on how innovations are forging the new landscape of the industry. At its core, the role is designed to strategically reshape the delivery of care.
Divya Paliwal, M.D., is chief transformation officer at Horizon Blue Cross Blue Shield of New Jersey (BCBSNJ). She graduated with honors from Johns Hopkins University and received her M.D. degree from Delhi University in India. Before coming to work as the CTO for BCBSNJ, Paliwal served as the vice president at Kaufman Hall & Associates.
At BCBSNJ, Paliwal works to make care more accessible to members across the Garden State. She helped establish a virtually integrated delivery network through the Omnia Health Alliance and is working to solve complex healthcare challenges and better serve the network’s members.
I recently caught up with her to learn more about how she’s using analytics and population health strategies to drive value in healthcare.
Editor’s Note: This interview has been slightly edited for length, clarity and style.
Samara Rosenfeld: What are your short- and long-term goals at BCBSNJ to drive improvement and value?
Divya Paliwal: We are focused on every component and element of the quadruple aim. There’s widespread discussion across the industry that the costs we will be seeing over the next several years are unsustainable. So is the basic model of a fee-for-service-driven healthcare industry. At Horizon, we have a responsibility to, and on behalf of, our members to strive for affordability. As we think about how we manage those costs, we are looking at a total cost of care and effort with our provider network. The value-based healthcare strategy is a linchpin to our strategic differentiation in the market and we're focused on driving that. It’s focused on how we align our provider network financially to work to achieve our total cost-of-care goals.
If there is one element in that quadruple aim that serves as the North Star for us, it’s quality. We firmly believe that if we are to drive sustainable improvement in overall population health long term, we need to drive improvements in quality and outcomes. As we think about how we are measuring quality, we are increasingly focused on evolving the definition of quality. We are focused on looking to move from a disease-centric siloed view to a comprehensive-centric view. Everything that is happening and the care that is being rendered to our members — how is it improving outcomes overall?
Experience is also critical. How can we drive seamlessness across the continuum of care, and how can we reduce friction points?
Around providing patient satisfaction, there is a lot of conversation around physician burnout. The way we address this is in a mindful manner. How can we use technology platforms and solutions to help make day-to-day activities and interactions easier? We are also working closely to align with organizations to reduce the administrative burden, policies and authorization requirements that create a lot of back and forth.
S.R.: Can you tell me about the healthcare value strategy at BCBS and the components that are driving it?
D.P.: From a healthcare value strategy perspective, when you think about cost, financial alignment with provider partners is absolutely critical and something we are working toward. Horizon has been working on value-based care for a number of years, but how do we expand that to a more advanced end of the spectrum where we are looking at upside and downside risk?
Around quality and clinical transformation, what we are working on internally and with the provider is on that integrated model. So physical health, behavioral health and social needs all need to come together. We have done a lot of work around developing these integrated systems in terms of bringing in behavioral health.
We have had a lot of success in our social determinants of care strategy. For example, we set up a pilot in 2017 that started in the Newark area for populations with access issues and who use the emergency room as their primary point of care. They have significant gaps in behavioral health access. We brought together our resources at Horizon, bringing one of our Omnia Alliance partners and community resources together to serve the needs of the population to look at the non-traditional needs of the members. We saw almost a 25% reduction in emergency department visits and more than 35% improvement in behavioral health access points, which is exactly what we wanted. And a reduction in total cost of care.
On the member experience front, how do we make this really complicated healthcare system simpler? Take scheduling. What we are working toward now with the platforms we have brought to the market. How do we make scheduling as simple as tapping a button on your phone? It’s that work and leveraging our deep relationships with our provider network to enable that.
S.R.: How do you leverage analytics to solve healthcare challenges?
D.P.: At Horizon, we have made significant investments, especially in the last few years, in our technology and analytics infrastructure and offerings. The presence and use of data are obviously not new, but what is more recent is the advances that we have seen in technology have helped us use data in a deeper and broader sense.
We have Health Sphere, a private health information exchange platform. We are using it to bring in all of the rich, clinical data that sit in the provider network, and we are marrying the information with the claims data available within Horizon and multiple third-party sources. We are combining it to get rich insights and broad data sets that we can harness to get information on how to manage the population.
It also improves the frequency because as you are thinking about managing population health, what’s important is that there is not a big lag in the data.
These investments help us become increasingly as near real-time as possible.
The other thing we are doing is looking at expanding applications. For example, we have information related to costs. We have information related to quality and access. Now how do we bring all of this together to provide a comprehensive snapshot of performance, and how do we share that in an action-oriented manner at the point of care? When you think about point of care, you think about how we embed that analytical information in terms of clinical decision support that providers can use when they are making clinical decisions.
S.R.: What is the virtually integrated delivery network and how was it established?
D.P.: The Omnia Alliance was launched in late 2016. The vision was to develop a statewide, optimized delivery network. As we thought about how to do that, there were several criteria we used to select our partners — right now we have seven, six of which are large health systems in New Jersey. The chief criterion was a philosophical alignment in terms of a focus on value-based care capabilities and a system scale that would serve to advance the capabilities and other aspects related to service.
We have key guiding principles that serve as the bedrock of the virtual network. Core among those is that care needs to be integrated. We are not going to silo physical health from behavioral health to social needs. Our provider partners have a central goal of managing population health, which includes truly managing the continuum of care and a heavy focus on infrastructure, which is through technology and analytics.
S.R.: How can other chief transformation officers stay on top of the ever-changing environment in healthcare?
D.P.: If you take a step back, we have been seeing advances in technology, and it is growing rapidly. Now combine that with biotech. The level of information that we are going to have around ourselves and bodies at the molecular and genomic level — it’s going to be a level of change that I think makes it difficult for anyone to anticipate what the future looks like.
Working in healthcare, there are direct implications for us and what we are going to be doing and serving in the future. There have been changes in how healthcare works in every which way.
With the level of complexity and change, one of the key things is for leaders, especially those focused on transformation, is to read, learn and network in increasingly eclectic manners. You cannot just be focused on siloes or your industry; it needs to be more broad to see what other applications exist.
Given the level of change, no one individual, team or organization can do it all. The role of collaboration and partnerships is going to be of increasing importance.
I believe that transformation needs to be deeply tied to execution, especially in a world where there is so much change. Otherwise, you are always looking for the next big idea. Ideas by themselves are not necessarily good or bad — it’s how you implement and execute them.
Get the best insights in digital health directly to your inbox.
More Executive Voice Interviews
