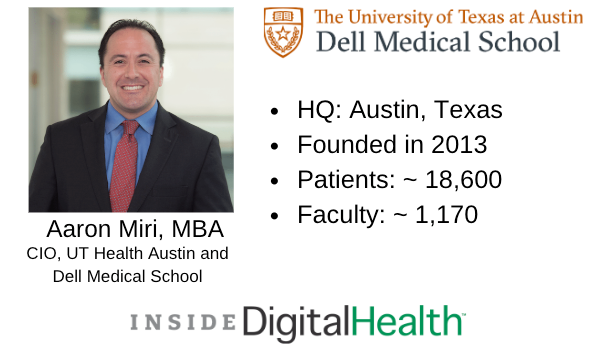
Executive Voices: Aaron Miri, MBA, CIO of UT Health Austin, Dell Medical School
He’s taking what he learned as a member of HITAC to help UT Health Austin stay ahead of new interoperability standards.
As health systems brace for new interoperability rules, members of the Health Information Technology Advisory Committee (HITAC) believe the proposed measures are a good first step. But some experts argue that true interoperability will require more action in the future.
Aaron Miri, MBA, is chief information officer (CIO) of UT Health Austin and Dell Medical School and a HITAC member. He’s also an expert adviser to the U.S. Senate Committee on Health, Education, Labor and Pensions and to other congressional panels engaged in health IT policy.
Miri is taking what he learns as a member of these organizations to better position UT Health Austin and Dell Medical School when the interoperability rules are finalized.
I talked with Miri about how health systems should prepare to implement new interoperability standards and how he embraces his roles at different organizations and leverages partnerships to better position UT Health Austin.
Miri is a graduate from the University of Texas at Arlington and received his Master of Business Administration from the University of Dallas. Prior to his work at UT Health Austin, Miri served as CIO for Imprivata where he helped build and transform a global commercial enterprise focused on healthcare cybersecurity.
Editor’s note: This interview has been lightly edited for length, clarity and style.
Samara Rosenfeld: How are you tackling interoperability at UT Health?
Aaron Miri: Interoperability is one of the most important aspects of what we provide from a health IT continuum and ecosystem perspective. If you look across the continuum of care, we have a close partnership for ambulatory care with Ascension Seton (another health system). We have close partnerships with all of the area hospitals here in Austin, Texas. We have patients and physicians who transition from various points of care.
Interoperability, to me, is about simplifying and making sure that a patient’s information is in the right place at the right time, with the right demographics and information attached to it. Then a clinician can make a decision without waiting or trying to search for information or being perplexed because they aren’t seeing the full picture.
We spend a lot of time with our partner organization making sure that our electronic health record (EHR) can speak with theirs. We have data repositories with our PACS images and other imagery that is easily transmittable from a care delivery perspective.
And then there’s research. University of Texas is world renowned for its research. We partner with many organizations across the globe. In the research dimension, interoperability is about making sure our researchers can collaborate and find new therapies and cures a lot faster and more effectively.
S.R.: I know you’re a member of HITAC. What’s on its radar as far interoperability recently?
Aaron Miri: HITAC is laser-focused on making sure we get the 21st Century Cures Act charges of interoperability and information blocking correct.
Within 21st Century Cures, if you in any way broker, deal or handle electronic protected health information from a patient, you cannot inhibit or prevent that information from being shared downstream with other providers or the patients. There’s a series of stipulated regulations that enable the Office of the National Coordinator of Health IT (ONC) to verify, validate and begin to penalize those who are not playing by the rules. The whole point of it is simple: Empower the patient to get their information whenever and however they want, effectively and reasonably. So HITAC is focused on making sure that is appropriately discussed and worked through.
The other dimension of this is the Trusted Exchange Framework and Common Agreement (TEFCA). The best way to imagine this is as a series of highways across the U.S. that allow large and small care providers to connect their data sources to enable that information to flow freely to a patient.
So if I live in Texas and find myself in Boston and have to go to a hospital, I can get my records without a problem, and caregivers can provide the best possible, most timely care. It’s all about empowering the patient, liberating the data and making sure all applicable laws and regulations are followed appropriately.
S.R.: How are you taking what you learn in government to fulfill your role as CIO at UT Health?
Aaron Miri: First of all, understanding the dynamics of what the law stipulates and the nuances behind it, making sure we can accomplish it. It’s helpful because in putting together notices of proposed rulemakings (NPRMs) and these rules, I can partner with our organizations and vendors in Austin to make sure that they’re aware of what’s coming down the pipe. I can also ensure that University of Texas is best positioned to continue enabling its mission of effective care, timely information and being the premier academic teaching environment across the globe.
From a healthcare delivery perspective, it’s all about preparation and making sure we are using constructs like application programming interfaces (APIs) and that our data are normalized and easy to access. It’s also about making sure our patients can easily access their data, which is why we partnered with Apple and launched HealthKit, so folks can download their medical records to their phones.
It’s all about making sure that we can pull every lever and are in compliance with the anticipated final ruling from these various NPRMs. It’s very helpful because it connects the dots. We’re not having to react. We are being proactive, and I can bring those learnings back to HITAC and say, “In working with our vendor community, we learned X, Y and Z. It may be helpful for us to consider this in our final rule.”
So it’s been a two-way street in bringing the theoretical down to reality and implementing it ahead of the curve, and then bringing that back to the discussion and saying, “Here are the learnings. Here’s what we can do.” And it’s been invaluable from our discussions perspective.
S.R.: What should health systems do to prepare to implement these standards?
Aaron Miri: No. 1, I would ask every health system and IT leader to read 21st Century Cures Act and understand what the law stipulates. There’s a tremendous amount of industry confusion based on the comments that have been received at the federal level for the NPRMs of, “What does information blocking actually mean?” “What does the TEFCA actually mean?” “What do all of the stipulations around the U.S. Food and Drug Administration actually mean?”
So, first off, seek to understand by reading what you’re supposed to do.
No. 2, partner closely with your vendor community and make sure your vendors are using common constructs like APIs — allowing data to freely flow. Make sure the contracts you signed with those vendors give you the ability to maneuver. And work with the vendors so that they can learn and understand how you wish to go about implementing it.
Last but not least, for any new contract you are negotiating, make sure the prospective vendor understands what’s coming down the pipe and what language you’re going to build into your contract to ensure enforceability of this.
Because at the end of the day — as a covered entity, as a hospital system or an academic health institution and teaching hospital — it’s incumbent upon us to make sure we lead the pack in partnering with the community to make sure they understand the importance of this and that we’re going to vote with our dollars. If a vendor doesn’t want to participate in liberating the data, then we are going in a different direction. And that’s the reality of what it’s going to take as health systems.
S.R.: What challenges can health systems expect to face?
Aaron Miri: Typical healthcare default mode is, “We’ve always done it this way, and we don’t want to change.” That’s going to be the most difficult thing because there are a lot of incredibly successful health institutions across the globe that have operated in the same manner for decades. Change doesn’t come easy in that situation.
If you look at what happened over the past decade with Meaningful Use implementation and the amount of churn that occurred in the industry because of that, these rules are the next level up on top of that. You can expect much of the same type of confusion, questions and lobbying once these go into final rule and the expected implementation occurs.
What I applaud the administration, the agencies and Congress for is the perspective of, “We will implement and we will free the data and make sure patients are empowered.” I wholeheartedly agree that it’s patient first always, and these rules were designed with the patient in mind.
S.R.: Why would health systems want to stick with what they know if they want seamless interoperability? Won’t this make their jobs easier and help them focus more on the patient?
Aaron Miri: Yes. I fundamentally believe people are in healthcare because they want to do good. It just gets very comfortable doing the same thing over and over again. And then suddenly when you have to change drastically because the industry has not been forced historically to share information, then there’s going to be normal change reluctance. I think any industry that is sort of flipped upside down and says, “Now you must,” has to go through a period of adjustment. That period will take some time.
Of course they want to change and do the right thing and liberate the data and improve outcomes, but change is tough and takes time. It behooves all of us to get on the horse and get going quickly rather than drag our heels and say, “I don’t want to change.”
S.R.: So are these rules enough to achieve nationwide interoperability?
Aaron Miri: No. HITAC does not believe that, and I don’t think the CIO believes that either. But this is a great first step. It’s not perfect by any means. I think the 21st Century Cures Act is an excellent step, but it’s not perfect. There will be future rulemaking on different aspects.
For example, how does HIPAA comply with information blocking and the TEFCA? There are a litany of state laws that are different than federal law when it comes to information security and privacy. So how do you reconcile that with a series of national highways for information? There are HIPAA challenges and data privacy laws that have challenges, depending on what state you’re in. Some states have taken it to the next level in terms of when you have to disclose a breach. How do you comply when your data go international? Because now you are touching on GDPR and the privacy shield.
There are other aspects that have to be addressed over time, and that’s not lost upon anybody. But we have to start somewhere. Just like with Meaningful Use and how, over time, it evolved into an industry-accepted standard — much too will information blocking, the TEFCA and others.
S.R.: How are you collaborating with clinicians and vendors to humanize tech and transform healthcare delivery for consumers, patients and providers at UT Health?
Aaron Miri: We aren’t here to do the same thing we’ve always done. We’re always looking for a better way to do it.
We built an ambulatory, multi-specialty practice with no waiting rooms. So what does that mean when you don’t have your traditional waiting rooms? You have to streamline all of your processes and make sure your intake processes are good to go. You’ve got to make sure your EHR vendor understands you don’t have waiting rooms.
It forces a series of standards, with the patient in mind, toward expedited delivery of care and value-based care where we have a care team approach, so a patient doesn’t have to bounce clinic to clinic. We are going to the patient with a multidisciplinary team to assess and triage the patient.
It requires collaboration with vendors on a totally different level than a traditional health system because you are forcing the conversation, saying, “This is what we do, and if you want to partner with us and modify your application and systems to match our workflow, that’s what it’s going to take.” And the vendor community has been very responsive about that. When I partnered with our EHR vendor and said we don’t have waiting rooms knowing that their system is designed with waiting rooms in mind, it’s a difficult conversation, but they made it happen.
Our patient-reported outcomes vendor went above and beyond to make sure they can seamlessly integrate with our workflow and the different types of patient surveys that would go out.
Every vendor has to play ball when an organizational tone is that, “This will be different, better and something that is not the norm.”
Get the best insights in digital health directly to your inbox.
Hear from More Executive Voices
Trent Haywood, M.D., J.D., CMO of BCBSA
Karen Murphy, Ph.D., R.N., Chief Innovation Officer of Geisinger
Healthy Bottom Line: The Trouble With SDOH Programs and the Secret to Improving Them
September 28th 2021Several problems exist with current programs that address social determinants of health (SDOH); however, a new social model aims to combat these issues and improve the programs’ effectiveness.














